Department of Radiation Diagnostics and Treatment
The Department focuses on providing specialised and cutting-edge radiosurgery treatment – interventional radiology (IR) care for patients with very early stage (BCLC 0), early stage (BCLC A) and intermediate stage (BCLC B) of hepatocellular carcinoma (HCC).
Hepatocellular carcinoma is one of the most difficult to treat with surgery. When it comes to determining treatment strategy for patients with Hepatitis C virus-associated HCC, it is important to take into account that liver cirrhosis can be a competing disease. HCC is a radiotherapy (including stereotactic) and chemotherapy resistant tumor. Therefore, surgery (resection and liver transplantation) and IR (transarterial chemoembolization and percutaneous energy-based ablation) are the only effective therapy methods. The past two decades have witnessed substantial progress in the development of IR technologies, which has significantly increased the survival of patients with very early, early and intermediate stages of HCC according to the BCLC classification.
Balakhnin PV, Shmelev AS, Shachinov EG. The role of surgical technologies in the treatment of virus-associated tumors on the example of hepatocellular carcinoma. Pract Oncol;2018(19:4):348-377.
Balakhnin PV, Shmelev AS, Shachinov EG. Percutaneous energy-based tumor ablation: principles, technologies, results. Pract Oncol;2016(17:3):129-153.
Percutaneous energy-based tumor ablation (PDF)
Our specialists use unique diagnostic technologies based on flat-detector computed tomography (FDCT).
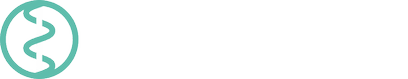
- Differential diagnosis of HCC nodules, dysplastic nodules, metastases, adenomas and cysts, along with foci of focal nodular hyperplasia by FDCT hepatic arteriography (FDCT-HA).
Fig. 1 Differential diagnosis of HCC nodules using FDCT-HA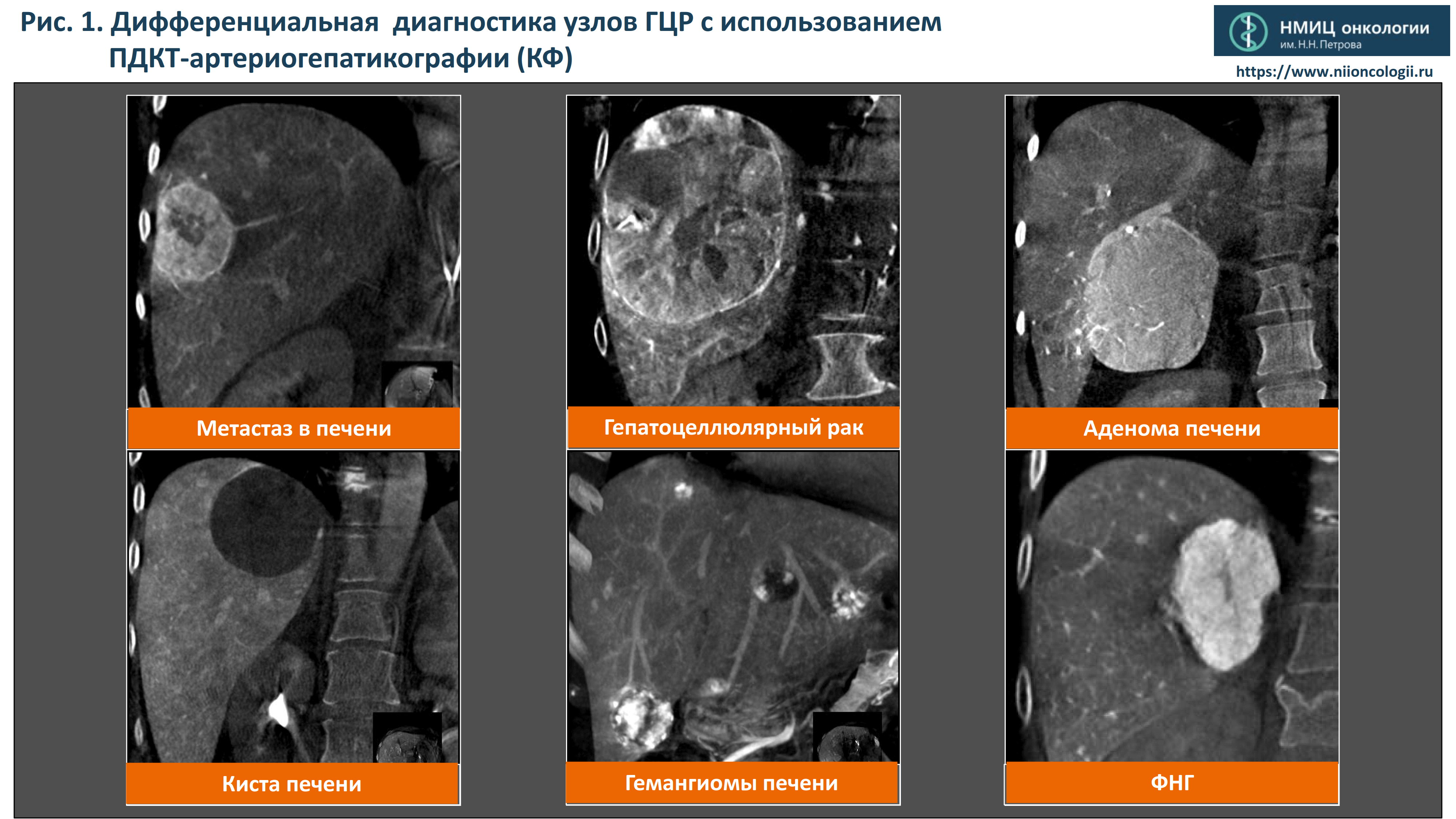
- liver metastasis
- hepatocellular carcinoma
- hepatic adenoma
- liver cyst
- hepatic hemangioma
- FNH
- Detection of additional multicentric HCC nodules (for patients with multifocal HCC), including nodules measuring less than 10 mm in diameter.
Fig. 2 Detection of additional multicentric HCC nodules during capillary phase of FDCT-HA.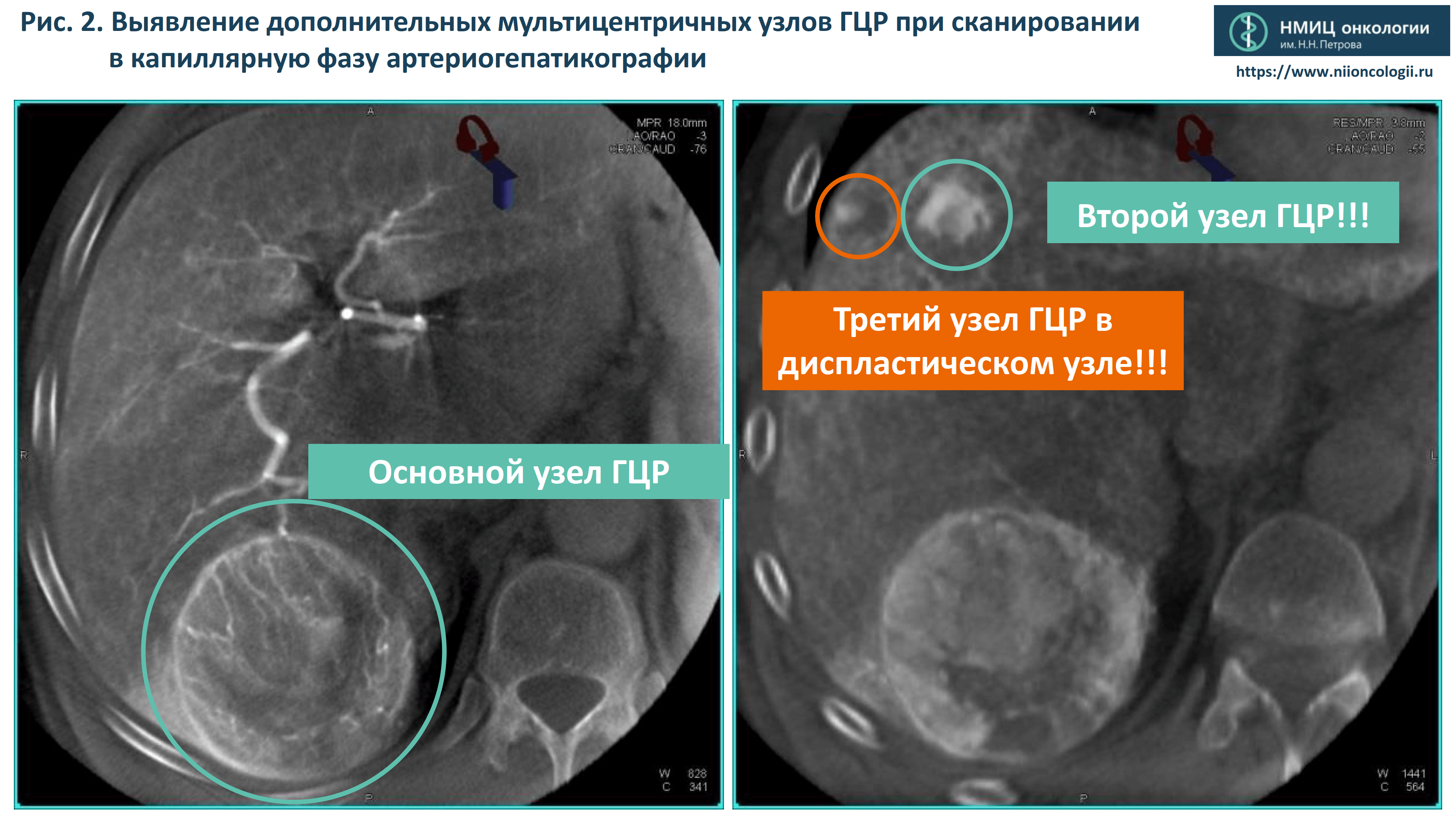
- main HCC nodule
- second HCC nodule
- third HCC nodule in the dysplastic liver nodule
- Assessment of invasion of adjacent organs and tissues by HCC nodules using FDCT arterial portography (FDCT-AP).
Fig. 3 Assessment of invasion of adjacent organs and tissues by HCC nodules: no invasions of the right kidney detected
- Diagnosis of intrahepatic HCC metastases, including those measuring less than 2 mm in diameter.
Fig. 4 Diagnosis of intrahepatic HCC metastases, including those measuring less than 2 mm in diameter: angiography and FDCT-HA comparison.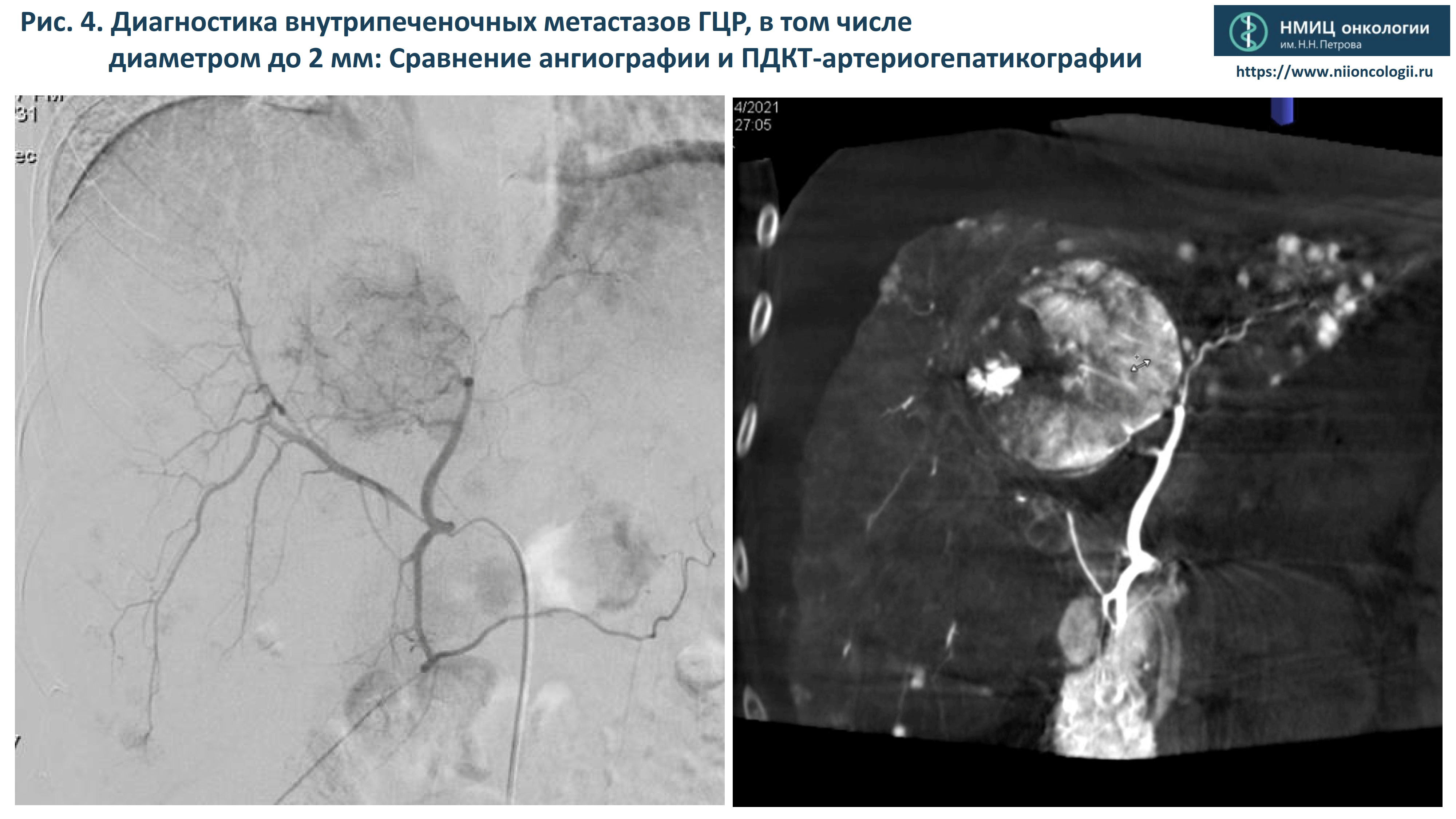
Fig. 5 Diagnosis of intrahepatic HCC metastases, including those measuring less than 2 mm in diameter.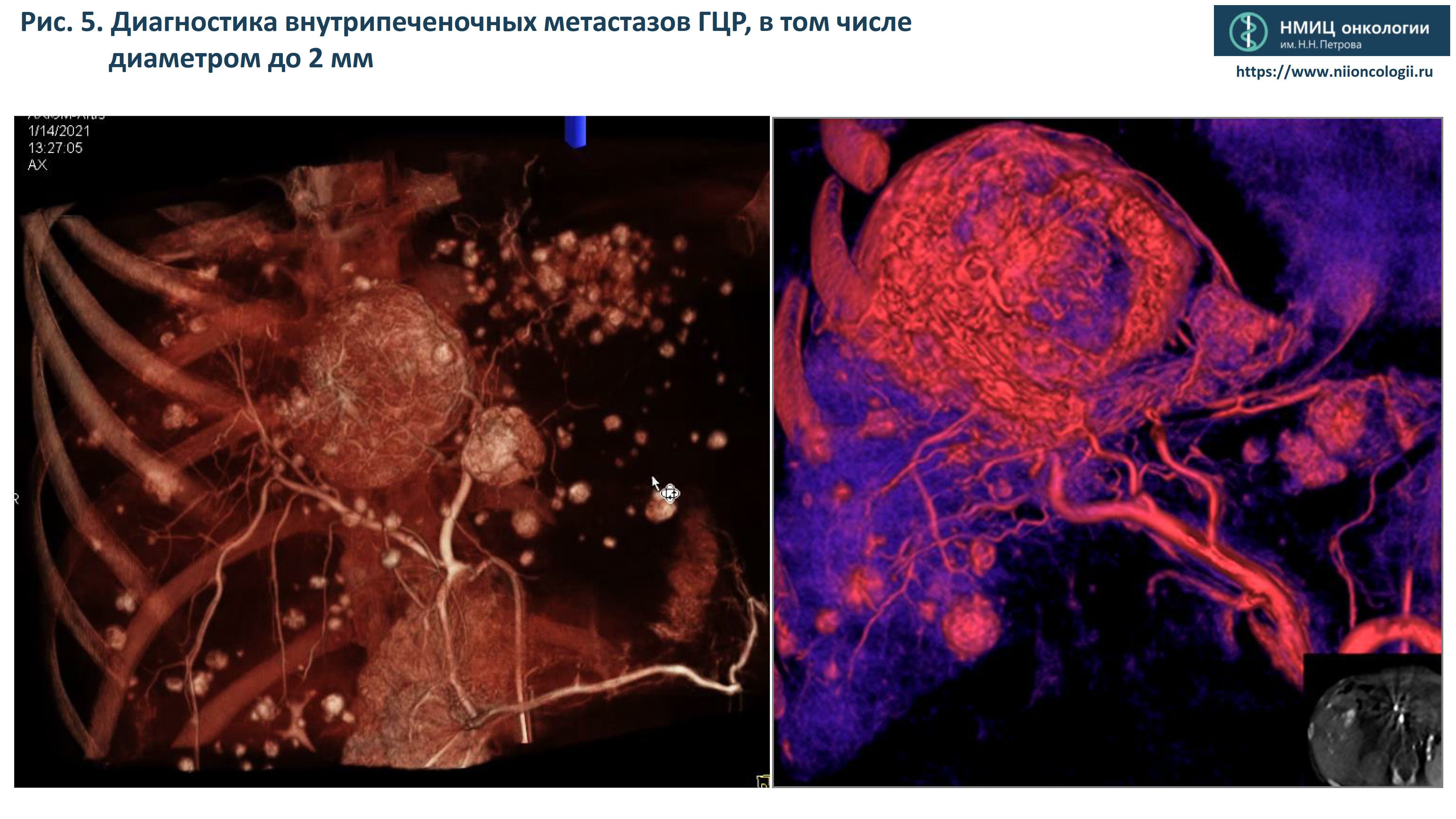
- Stereotactic angiography-assisted FDCT-controlled biopsy of tumours up to 10 mm in diameter using FDCT-HA technologies
Fig. 6a Unique opportunity to visualise 7 and 10 mm HCC nodules located in dysplastic nodules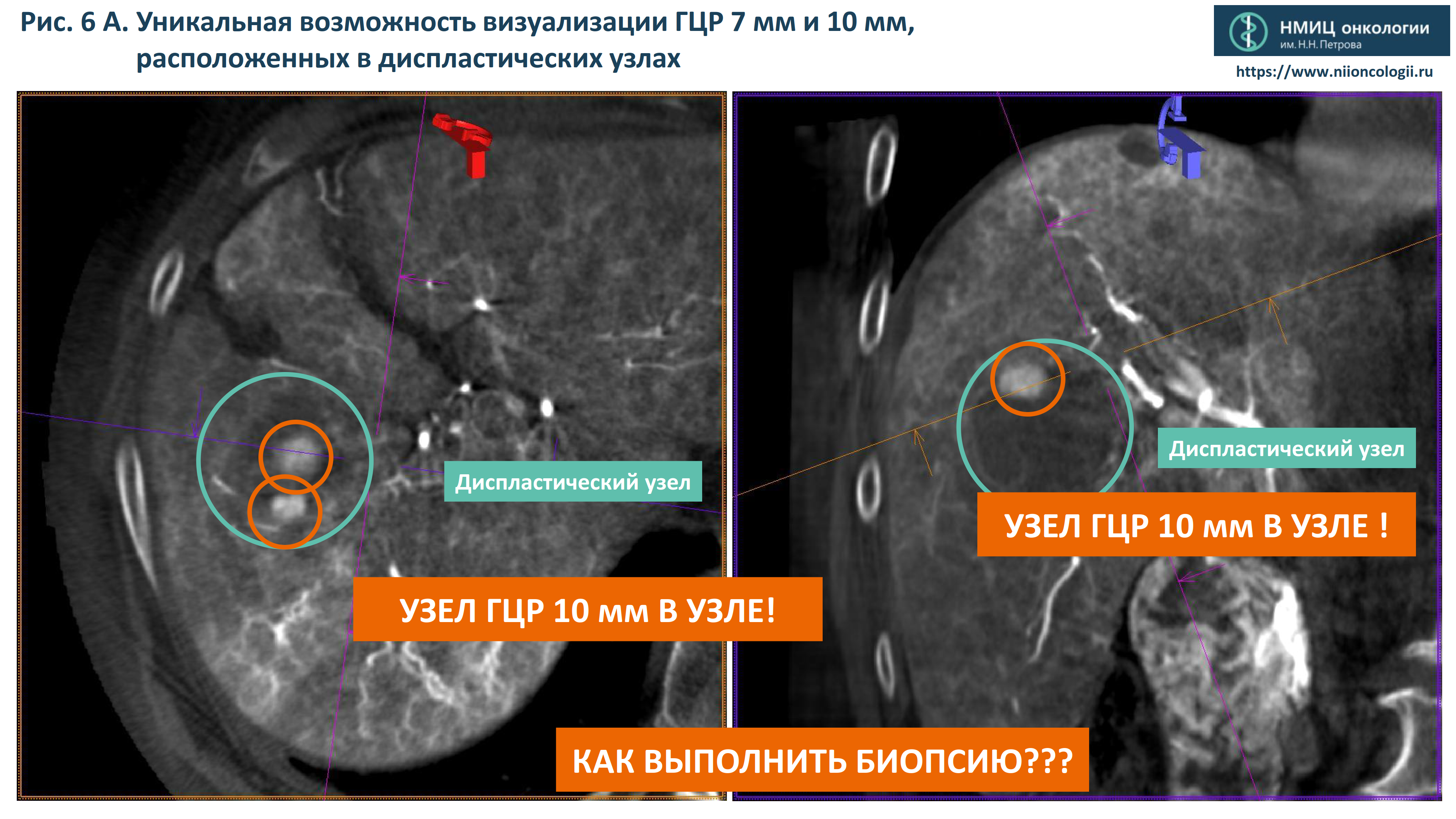
- Dysplastic nodule
- 10 mm HCC in dysplastic nodule
- How to perform biopsy?
Fig. 6b Stereotactic angiographic-assisted FDCT-controlled biopsy of 10mm HCC nodule.
- Tumour sample collection confirmed! + Full control of bleeding
- Stereotactic angiographic-assisted biopsy of very large tumors with lysis sampling of viable tissue under FDCT-HA.
- Assessment of Parenchymal blood volume (PBV) of HCC nodules with assessment of perfusion parameters of the tumour and cirrhosis-damaged liver parenchyma.
Fig. 7 Perfusion Blood Volume (PBV) study of HCC nodules with assessment of perfusion parameters of the tumour and cirrhosis-damaged liver parenchyma.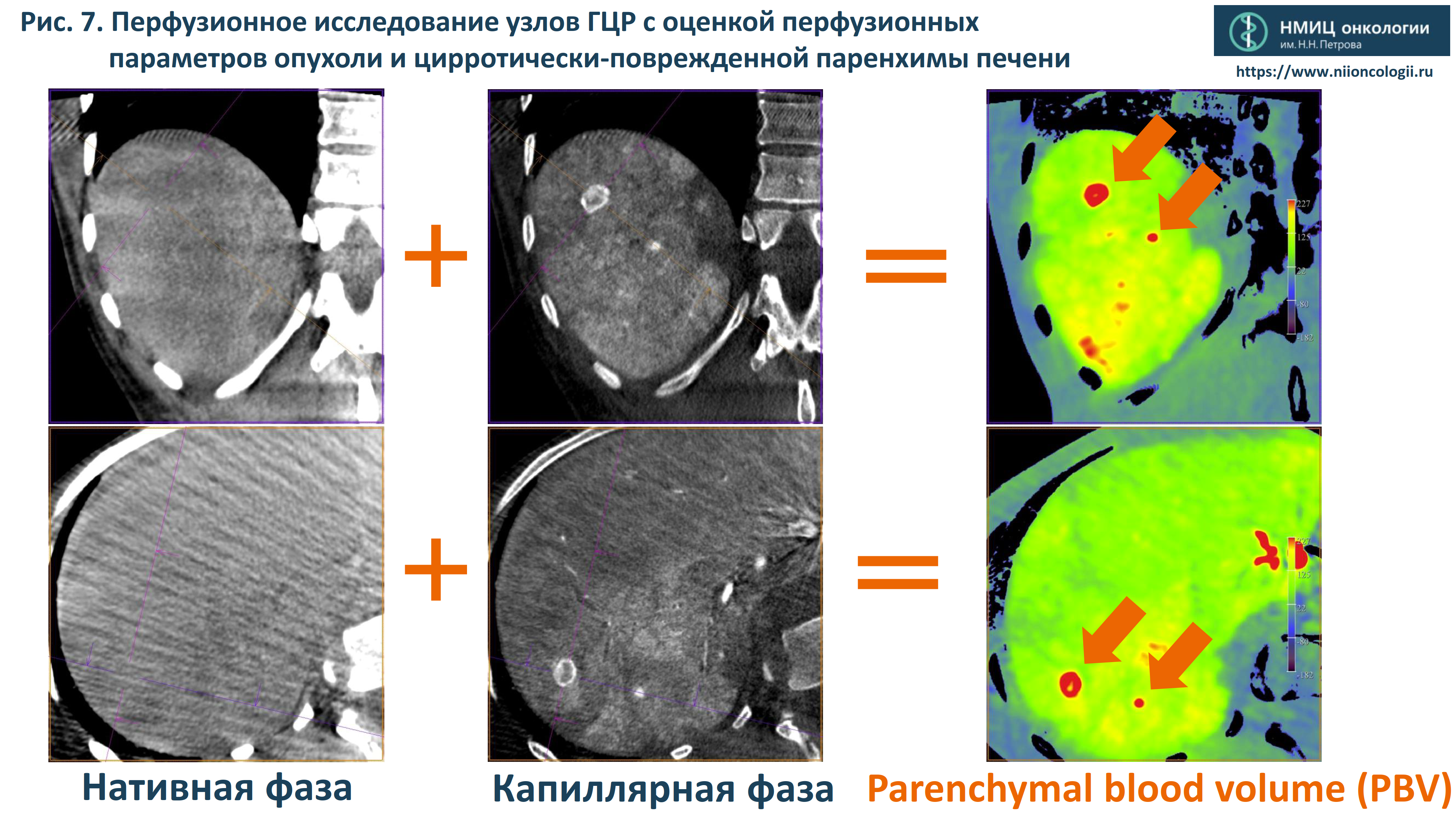
- Native phase
- Capillary phase
- Parenchimal Blood Volume (PBV)
- Tumour volume estimation and automatic search for tumour-feeding vessels before performing superselective transarterial chemoembolisation (TACE) of HCC nodules.
Fig. 8 Tumour volume estimation and automatic search for tumour-feeding vessels before performing superselective TACE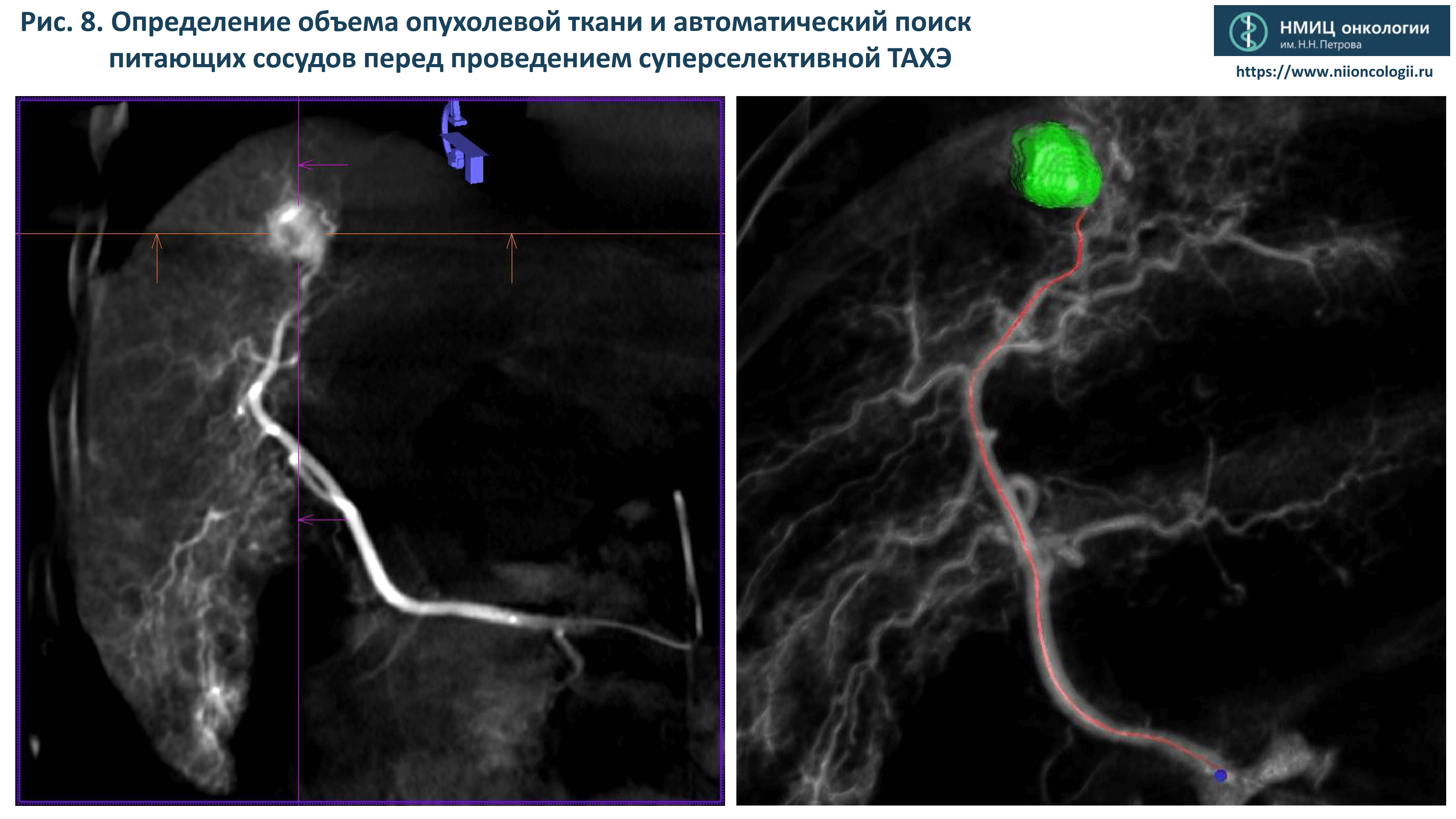
Our unique therapeutic technologies
- FDCT-controlled superselective transarterial chemoembolisation of tumour nodules using drug-saturated microspheres achieves complete tumor necrosis in a single session.
Fig. 9 FDCT-controlled superselective TACE allows to achieve complete HCC nodules necrosis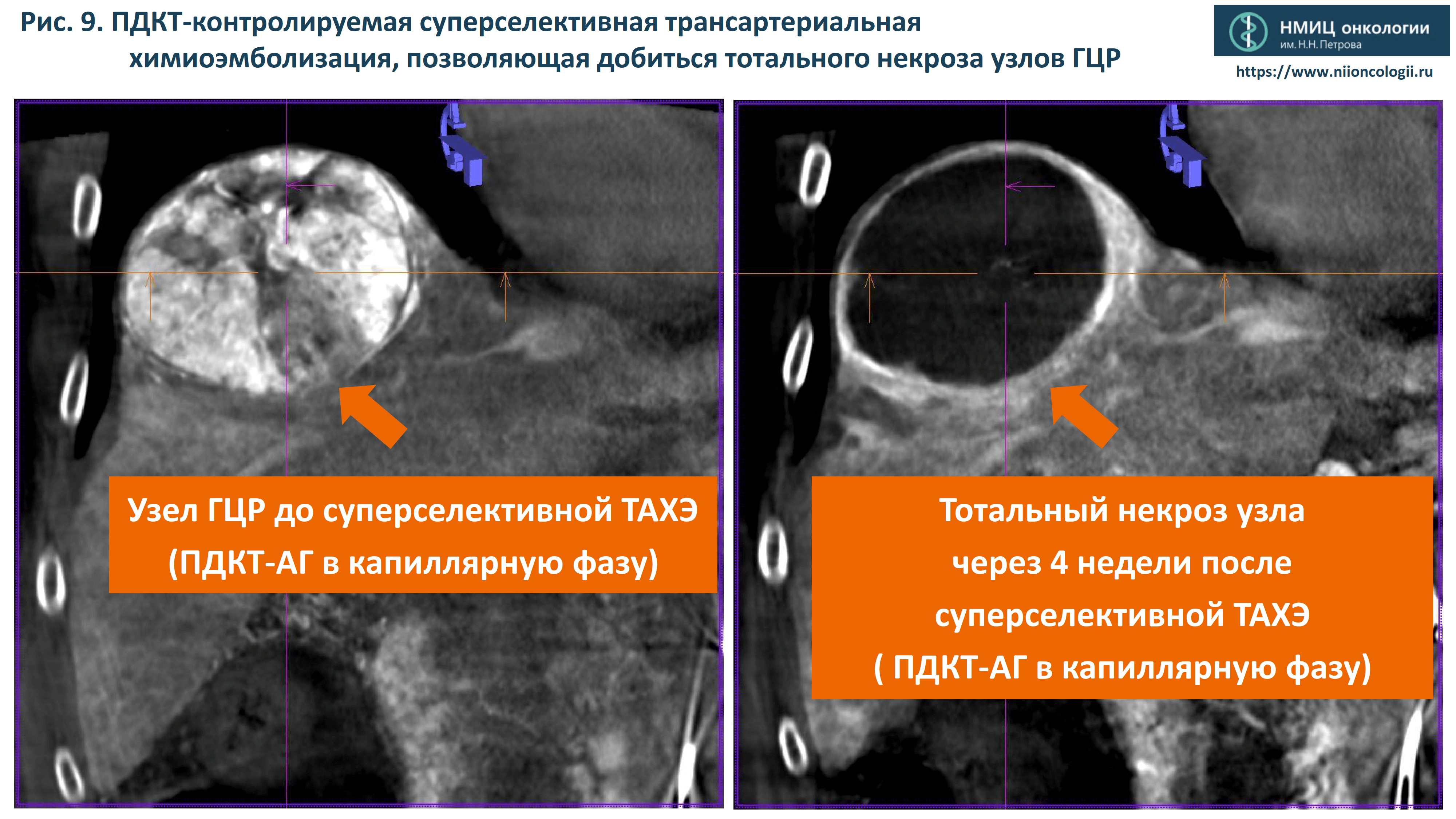
-
HCC nodule before superselective TACE
FDCT-HA in a capillary phase - Complete HCC nodule necrosis in 4 weeks after superselective TACE (capillar-phase FDCT-HA)
-
HCC nodule before superselective TACE
- Evaluation of chemotherapeutic drug accumulation in the tumour after TACE.
Fig. 10 Evaluation of chemotherapeutic drug accumulation in the tumour after TACE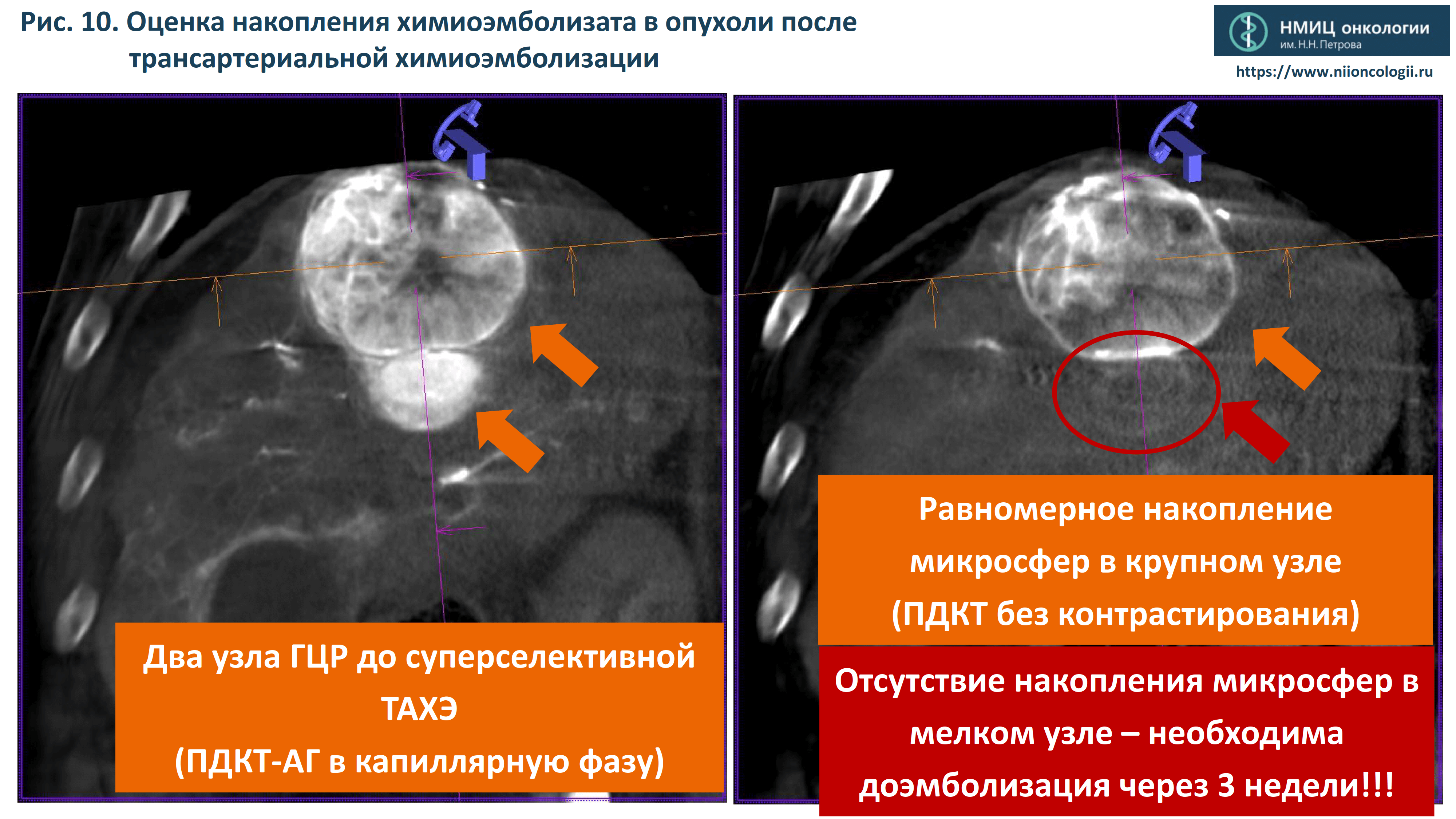
- Two HCC nodules before superselective TACE (capillar-phase FDCT-HA)
- drug-saturated microspheres Uniform accumulation of microspheres in a large nodule (non-contrast FDCT)
- No accumulation of microspheres in the small nodule - additional embolisation required after three weeks!
- A two-stage liver perfusion imaging before and after chemoembolisation to provide prognostic tumor treatment response markers.
Fig. 11 A two-stage liver perfusion imaging allows to predict tumour response to treatment immedeately after TACE is performed.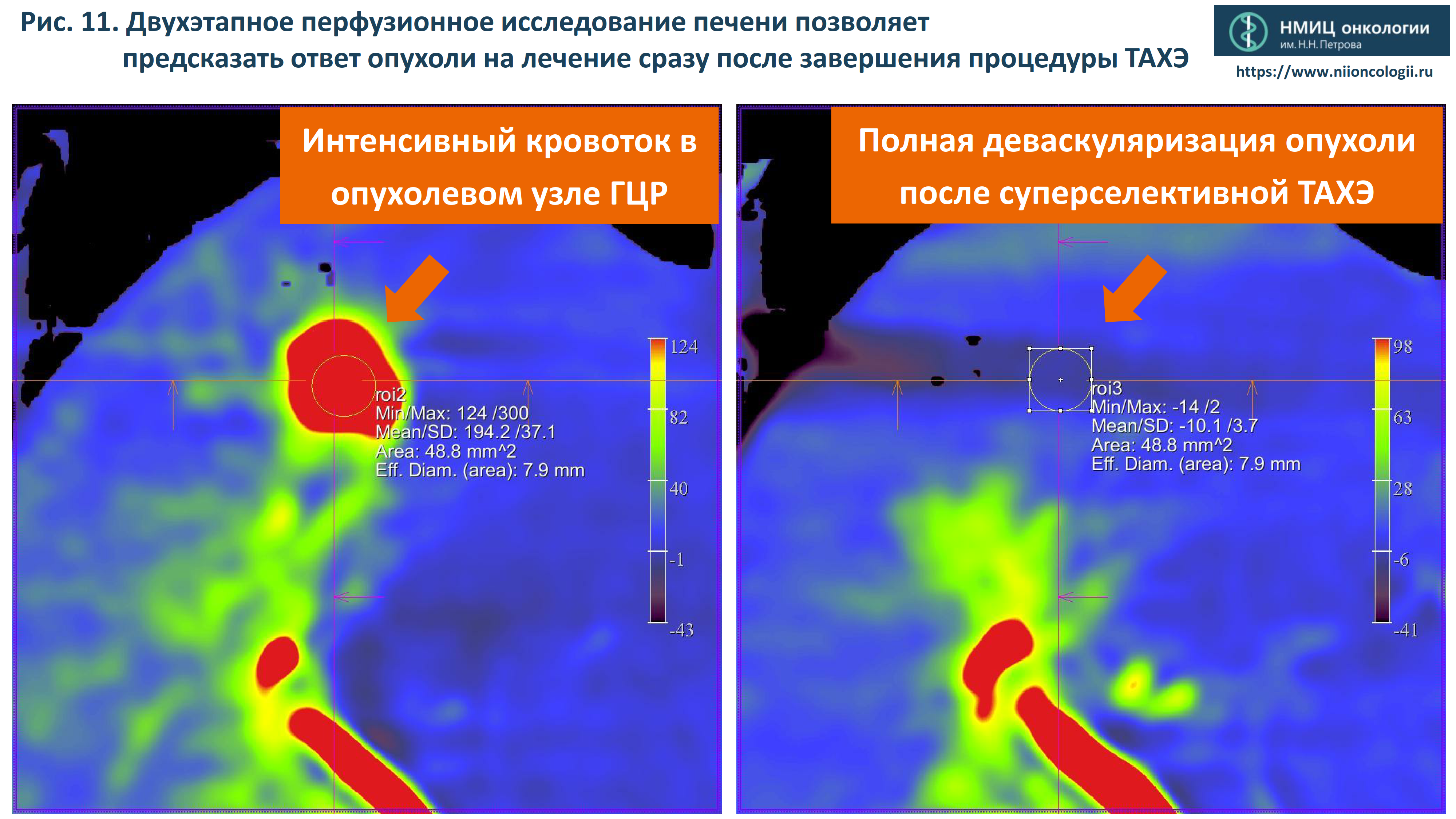
- Intensive blood flow in the HCC tumour nodule
- Сomplete tumour devascularisation after superselective TACE
- Angiography-assisted FDCT-controlled thermal ablation (microwave ablation, cryoablation) of HCC nodules to achieve radical tumour destruction within healthy tissue.
Fig. 12 Angiography-assisted FDCT-controlled microwave ablation (MWA) of two HCC nodules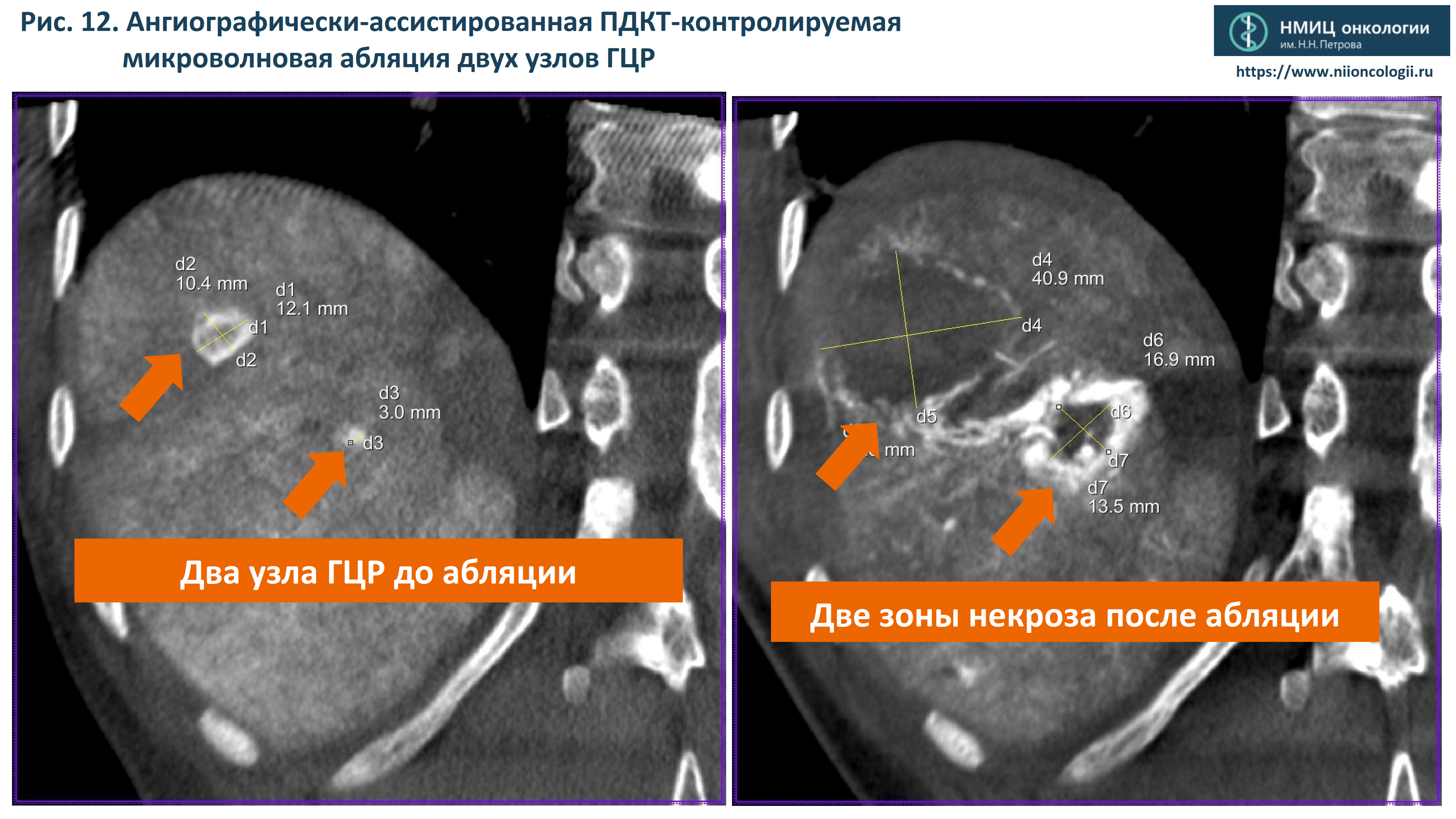
- Two HCC nodules before ablation
- Two necrosis zones after ablation
- Using image fusion techniques (FUSION) to assess the ablation margin as a prognostic factor for the radicality of the intervention.
Fig. 13 Using FUSION to assess the ablation margin as a prognostic factor for the radicality of the intervention (minimal ablative margin (MAM) > 10 mm)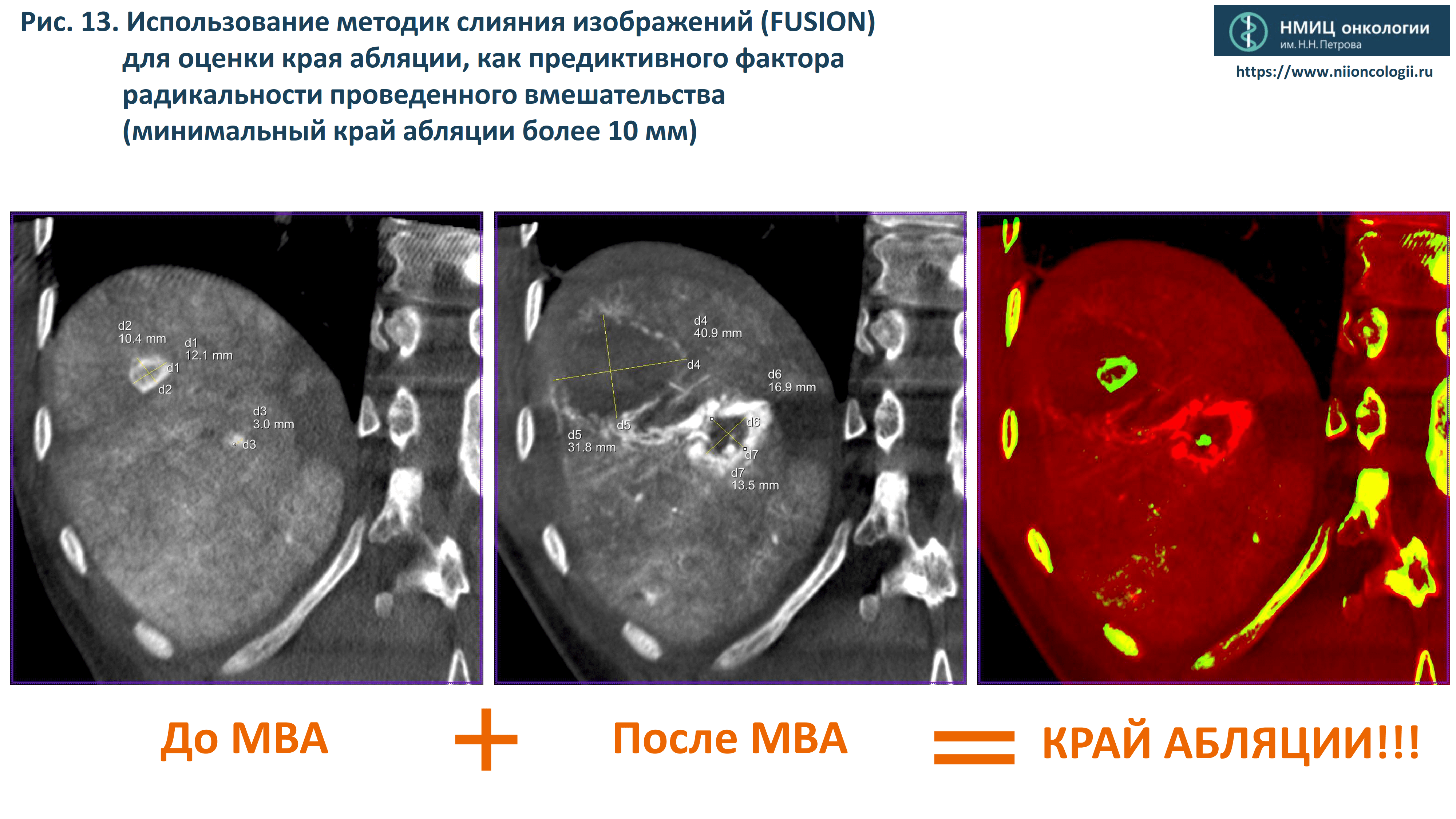
- Before MWA + After MWA = ABLATIVE MARGIN!
- Combined interventions involving TACE and percutaneous thermal ablation.
Fig. 14 Combined interventions: superselective TACE + percutaneous ablation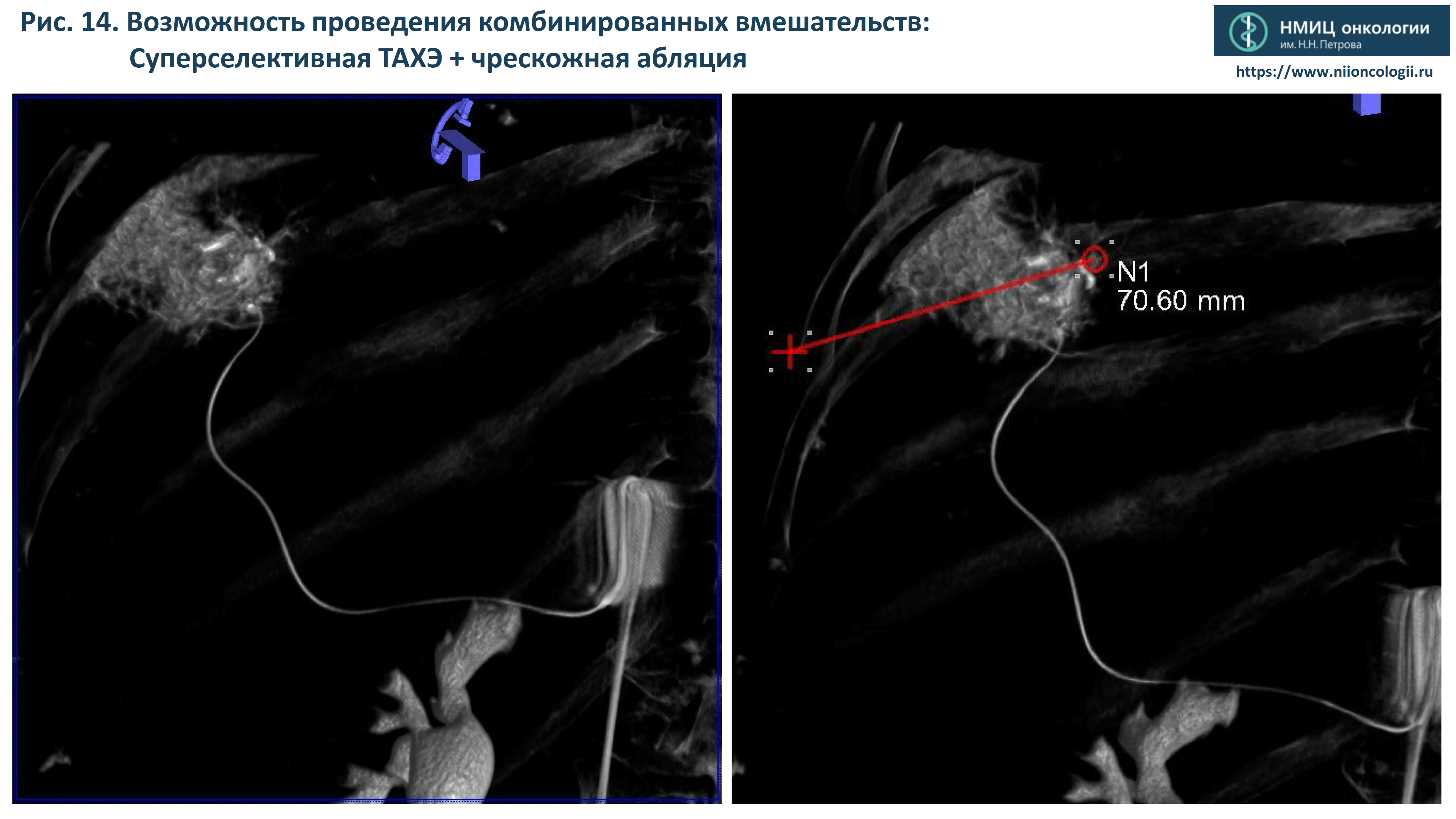
Our team is constantly working on streamlining the algorithms for the early diagnosis and treatment of hepatocellular cancer.
We work closely with experts from the related fields and participate in events to raise public awareness of HCC.